Abstract
Salivaomics has exciting potential for the diagnosis and monitoring of malignancy, evidence of which has been reported in oral cancer (Sahibzada et al., 2017), head and neck malignancies (Citrin et al., 2012) and ovarian cancer (Chen et al., 1990). It has been observed that approximately 40% of cancer, stroke and cardiovascular disease biomarkers are present in whole saliva (Loo et al., 2010). Salivaomics has become an area of great interest in disease diagnosis over the last number of years, following the footsteps of the other "omics" based diagnostic tools. Saliva has been referred to as "the mirror of the body" as it gives an insight into the internal pathological state (Lee and Wong, 2009). As saliva is considered a fast, inexpensive and non-invasive method of sample collection, the future of diagnosis, early detection, monitoring and prediction of progression of disease has been thought to lie here.
Monoclonal gammopathy of undetermined significance (MGUS) is characterised as a premalignant precursor tumours of MM. It has been seen that the majority of MM cases develop from MGUS (Weiss et al., 2009), leading to the need for biomarkers to monitor disease progression and explore the mechanism of malignant transformation.
Serum and saliva samples were collected from 18 newly diagnosed MM patients and 8 MGUS patients, peptides were purified using the filter aided sample preparation (FASP) method and samples were prepared for label-free liquid chromatography mass spectrometry (LC-MS/MS) using an LTQ Orbitrap XL mass spectrometrer (Thermo Fisher Scientific). Proteins were analysed using the MaxQuant and Perseus software for mass-spectrometry (MS)-based proteomics data analysis, UniProtKB-Swiss Prot database and KEGG Pathway database.
The abundance of proteins in saliva from MGUS compared to newly diagnosed MM was analysed using label-free mass spectrometry. A panel of 6 significant proteins was identified. Fatty Acid Binding Protein 5 (FABP5) was detected in elevated levels in saliva from MM patients compared to MGUS. The increased expression was verified using western blotting. Fatty Acid Binding Protein 5 (FABP5) is known to promote cell proliferation, survival and migration (Wang et al., 2006). FABP5 has been observed to aid in the proliferation of cancer and has been seen to be overexpressed in multiple cancer types such as breast (Levi et al., 2013), prostate (Morgan et al., 2008) and HCC (Ohata et al., 2017). FABP5 has seen to link closely with poor outcome and unfavourable clinical parameters in MM (Waheed et al., 2013).
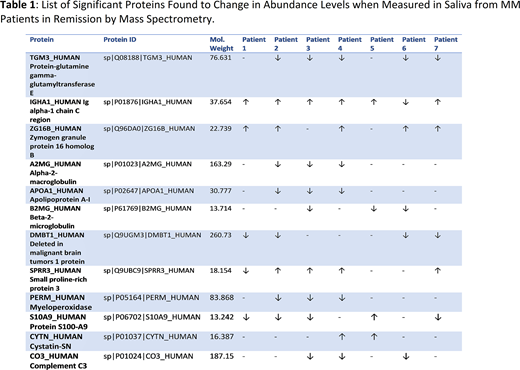
Additionally, analysis was performed on serial MM patient saliva samples during treatment. A panel of significant proteins was identified when comparing the saliva proteome during treatment the abundance of many of the detected proteins mirrored response to treatment (Table 1). For example, Transglutaminase 3 (TGM3) was observed as being decreased in abundance in saliva from patients in remission. TGM3 is expressed in brain, small intestine, mucosa and skin and has been shown to be required for the cross-linking of the structural protein trichohyalin and the keratin intermediate filaments to form a rigid structure within the inner root sheath cells (Hitomi, 2005). Overexpression of TGM3 has been observed to induce oesophageal cancer (EC) cell invasion, migration and proliferation. It has also been noted that TGM3 promotes apoptosis in EC in vitro (Li et al., 2016). TGM3 has been predicted to be a potential biomarker for disease progression in MM.
This study provides proof of concept that a range of biologically significant proteins of interest can be reliably detected in the saliva of MM and MGUS patients. The observation of differential expression of FABP5 between MGUS and MM identified these as candidate proteins relevant to malignant transformation of MGUS to symptomatic MM. The demonstration of decreased abundance of FABP5 after achieving remission indicates a correlation with tumour burden. This opens the opportunity to explore candidate salivary biomarkers for use in the clinic for disease monitoring and Minimal Residual Disease (MRD) assessment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal